A move by The Ottawa Hospital to promote less invasive surgeries for women with severe gynecological problems has sped up patient recovery, led to fewer complications and saved the hospital money, according to a study recently published in the Journal of Obstetrics and Gynaecology Canada.
In 2007, The Ottawa Hospital decided to become a national leader in minimally invasive surgery (MIS), a technique that uses tiny cuts instead of the large ones used in traditional open surgery. Researchers from The Ottawa Hospital and the University of Ottawa found the hospital's investment in MIS expertise and equipment made a big difference when it came to hysterectomies, a surgery to remove the uterus.
Hysterectomies are the most common surgery for Canadian women after the C-section. In 2012 more than 40,000 women had their uterus removed, usually due to serious non-cancer conditions like excessively heavy periods or painful growths called fibroids.
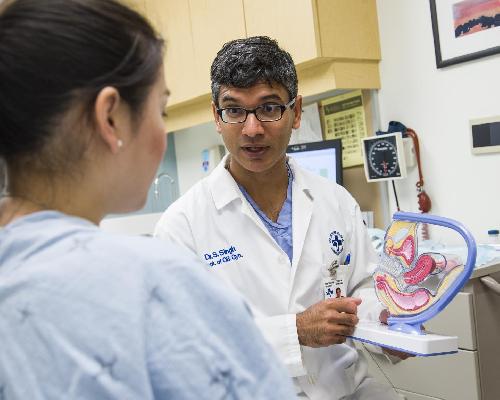 A move by The Ottawa Hospital to promote less invasive surgeries for women with severe gynecological problems has sped up patient recovery, led to fewer complications and saved the hospital money, according to a study recently published in the Journal of Obstetrics and Gynaecology Canada. Dr. Sony Sukhbir Singh, the senior author, is Vice-Chair, Gynecology, of the Department of Obstetrics and Gynecology at The Ottawa Hospital and the Elaine Jolly Research Chair in Gynecologic Surgery and an associate professor at the University of Ottawa Credit: The Ottawa Hospital
A move by The Ottawa Hospital to promote less invasive surgeries for women with severe gynecological problems has sped up patient recovery, led to fewer complications and saved the hospital money, according to a study recently published in the Journal of Obstetrics and Gynaecology Canada. Dr. Sony Sukhbir Singh, the senior author, is Vice-Chair, Gynecology, of the Department of Obstetrics and Gynecology at The Ottawa Hospital and the Elaine Jolly Research Chair in Gynecologic Surgery and an associate professor at the University of Ottawa Credit: The Ottawa Hospital
Traditionally hysterectomies are done through a large cut in the abdomen, and women who undergo this surgery can spend three to four days in hospital and six to eight weeks recovering. But for MIS hysterectomies, the half-centimeter-long incisions mean women can often go home within 24 hours.
"Patients who have had a minimally invasive hysterectomy are often surprised by the quick recovery and minimal pain," said senior author Dr. Sony Sukhbir Singh, Vice-Chair, Gynecology, of the Department of Obstetrics and Gynecology at The Ottawa Hospital and the Elaine Jolly Research Chair in Gynecologic Surgery.
"They can often recover from the operation without using painkillers," added Dr. Singh, who is also an associate professor at the University of Ottawa. "To be able to see that compared to the open hysterectomy, it's night and day."
D. Singh's study of 4,300 non-cancer hysterectomy patients treated at The Ottawa Hospital from 2005 to 2012 showed the hospital's investments in MIS expertise and equipment have paid off. In 2005, 40 percent of the hysterectomies performed at The Ottawa Hospital were minimally invasive. By 2012, that number had jumped to 74 percent.
"What we found was amazing. We've basically changed the way we practice," said lead author Dr. Jenna Gale, an Obstetrics and Gynecology Resident at The Ottawa Hospital and the University of Ottawa. "The most common surgery used to be done through a big cut. Today we've completely flipped that, and now the most common routes for hysterectomies for women are minimally invasive throughout The Ottawa Hospital."
The study also found that MIS patients had fewer blood transfusions, bowel problems and blood clots than the traditional hysterectomy patients. The average of stay in hospital also decreased from 2.5 to 1.6 days, saving 1898 inpatient bed days. These quicker recovery times meant the hospital was able to free up eight beds across the gynecology wards for other kinds of surgeries.
"Today women are getting the best type of surgery done, with the least amount of complications," said Dr. Mark Walker, head of the Department of Obstetrics, Gynecology and Newborn Care at The Ottawa Hospital and professor at the University of Ottawa. "From the patient perspective it means less pain, quicker recovery, and quicker return to work or normal activities. It's an incredible benefit to them."
For the last 10 years, medical guidelines have recommended surgeons choose minimally invasive hysterectomy whenever possible. However, adoption of this practice has been slow in Canada, where 54 percent of hysterectomies were performed abdominally in 2008.
Dr. Singh says barriers to more doctors adopting MIS hysterectomies include lack of training, the perceived difficulty of the procedure and the cost of the equipment. However, their study found that while MIS equipment might initially cost more, the procedure itself costs less. On average a traditional hysterectomy costs the hospital $7,200, while the less invasive vaginal and laparoscopic methods cost $4,500 and $5,600 respectively. Dr. Singh estimates that MIS hysterectomies save the hospital about $200,000 a year.
Considering the benefits of MIS hysterectomies, Dr. Singh hopes they will become more widespread across Canada, and that more women will request the procedure.
"I just hope that we can see this happen around the country at a larger scale," said Dr. Singh. "The willingness is there, but we need to encourage others to adopt minimally invasive techniques."
source: Ottawa Hospital Research Institute