New research helps bridge an important gap in understanding schizophrenia, providing the best evidence to date that defects in the brain's white matter are a key contributor to the disease, which affects about 1 percent of people worldwide. The findings, to be published online by the Proceedings of the National Academy of Sciences during the week of April 23, also demonstrate how two of the dozen or more genes previously linked with schizophrenia may contribute to the disease.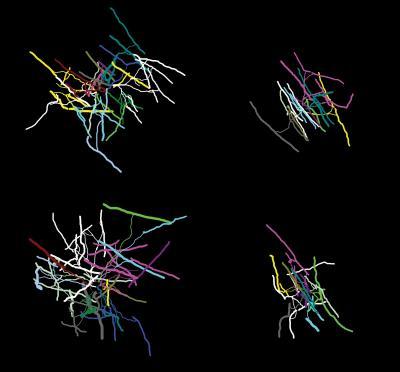 When NRG1-erbB signaling was blocked, oligodendrocytes from the brain's frontal cortex had a less complex structure than normal, forming fewer branches. Shown are three-dimensional reconstructions of oligodendrocytes from a normal mouse (left) and a mutant mouse (right). Credit: Image courtesy Joshua Murtie, Ph.D., Children's Hospital Boston.
When NRG1-erbB signaling was blocked, oligodendrocytes from the brain's frontal cortex had a less complex structure than normal, forming fewer branches. Shown are three-dimensional reconstructions of oligodendrocytes from a normal mouse (left) and a mutant mouse (right). Credit: Image courtesy Joshua Murtie, Ph.D., Children's Hospital Boston.
Prior genetic studies had linked schizophrenia to the genes for neuregulin 1 (NRG1), a growth factor involved in brain development, and erbB4, a receptor on brain cells through which NRG1 exerts its action. But until now it hadn't been shown that alterations in these genes lead to psychiatric disorders. Working in a mouse model, researchers led by Gabriel Corfas, PhD, Kristine Roy, PhD, and Joshua Murtie, PhD, in the Children's Hospital Boston Neurobiology Program now demonstrate, for the first time, that alterations in NRG1-erbB signaling induce pathologic changes in the brain's white matter. They further show that these changes lead to alterations in biochemical signaling and to behaviors suggestive of mental illness.
"We show that causing a defect in white matter is sufficient to cause biochemical and behavioral changes resembling those seen in neuropsychiatric disorders," says Corfas, the study's senior author. "I think this will provide a new way of thinking about the causes of, and possibly, therapies for schizophrenia."
The findings could also have implications for bipolar disorder, which has also been linked with NRG1 and also involves white matter defects, he adds.
Working with mice, the researchers blocked NRG1-erbB signaling in oligodendrocytes –the cells that form the fatty sheath, known as myelin, which insulates nerve fibers. These myelinated nerve fibers make up the brain's white matter. When NRG1-erbB signaling was blocked, the mice had more oligodendrocytes than normal mice, but these cells had fewer branches and formed a significantly thinner myelin sheath around nerve fibers. As a result, the nerve fibers conducted electrical impulses more slowly, the researchers found.
The mice also had changes in the nerve cells that make and use dopamine, a key chemical in the brain that transmits messages from one nerve cell to another. The dopamine system has long been known to be altered in schizophrenia, and is the target of many antipsychotic drugs.
"Changing the white matter in the brain apparently unbalanced the dopamine system, something that also occurs in patients with neuropsychiatric disorders," says Corfas.
Finally, mice whose NRG1-erbB signaling was blocked showed behavioral changes that appeared to be consistent with mental illness. They explored their environment less than normal mice and had reduced social interaction, thought to be a manifestation of so-called "negative" schizophrenic symptoms such as decreased initiative and social withdrawal. The mice also showed behaviors suggestive of anxiety, a symptom seen in patients with schizophrenia and bipolar disorder, and increased sensitivity to amphetamine, also seen in many schizophrenia patients.
Is it possible to modify NRB1-erbB signaling with drugs, or otherwise protect oligodendrocytes (and white matter) as a way of treating or preventing schizophrenia?
"This is something that should be investigated," says Corfas. "People are thinking about ways to repair white matter as a treatment for multiple sclerosis, which is also a disease of white matter. That research could now be used in thinking about neuropsychiatric disorders."
Schizophrenia is typically diagnosed in late adolescence or early adulthood, but it is almost always preceded by subtle affective, cognitive or motor problems, Corfas adds. "We need to investigate whether the white-matter defects emerge early, before psychotic symptoms are evident," he says. "If they do, that raises the possibility of early diagnosis and preventive treatment."
The idea of schizophrenia arising from white-matter defects may also help explain the timing of its emergence, Corfas notes. Recent evidence suggests that myelination of the prefrontal cortex (a brain area that has been implicated in schizophrenia) occurs not only during infancy and toddlerhood, but also during late adolescence or early adulthood – just when schizophrenia strikes.
"We now need to go back to patients with schizophrenia and see whether those with variants of the NRG1 and erbB4 genes have differences in their white matter," Corfas says. "It may be that there are different kinds of schizophrenia, arising from alterations in different genes, and that directed treatments could be developed for the different forms."
Corfas and colleagues also plan to investigate other genes linked with schizophrenia, studying whether they interact with NRG1-erbB signaling and how they may alter brain function.
Source: Children's Hospital Boston.