University of California, Berkeley, biologists have discovered the switch that triggers the power kick sperm use to penetrate and fertilize a human egg, uncovering a possible source of male infertility but also a potential target for contraceptives that work in both men and women.
The switch is a protein receptor that responds to the female sex hormone progesterone, which is released by the egg or oocyte, the ultimate goal toward which sperm swim. Thousands of these receptors sit on the surface of a sperm's tail and when the sperm gets close to the egg, the hormone activates the receptor and triggers a cascade of changes that make the tail snap like a whip, powering the sperm into and hopefully through the cells protecting the egg.
"If the receptor protein doesn't recognize progesterone, you would be infertile," said Melissa Miller, a postdoctoral fellow at both UC Berkeley and UC San Francisco and the first author of a paper reporting the discovery. "This gives us an understanding of another pathway that is involved in human sperm activity."
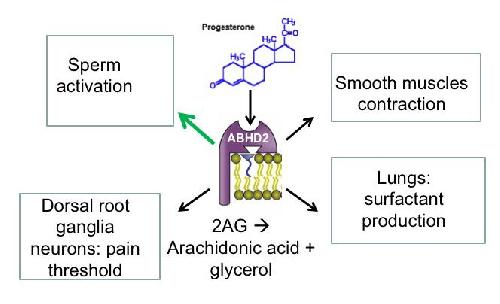 Progesterone, a sex hormone involved in all aspects of female fertility, also primes sperm make the final push toward fertilizing the egg. UC Berkeley researchers have discovered the receptor -- the protein ABHD2 -- that responds to progesterone on sperm cells and initiates the power kick of the sperm's tail that propels it into the egg. This receptor is found in many other tissues, and may be the key relay in progesterone's actions on nerve cells, smooth muscle and lung tissue. Credit: Polina Lishko and Melissa Miller, UC Berkeley
Progesterone, a sex hormone involved in all aspects of female fertility, also primes sperm make the final push toward fertilizing the egg. UC Berkeley researchers have discovered the receptor -- the protein ABHD2 -- that responds to progesterone on sperm cells and initiates the power kick of the sperm's tail that propels it into the egg. This receptor is found in many other tissues, and may be the key relay in progesterone's actions on nerve cells, smooth muscle and lung tissue. Credit: Polina Lishko and Melissa Miller, UC Berkeley
A drug that inactivates this newly discovered receptor, however, might make a good "unisex" contraceptive -- one that could be used by either sexual partner.
"What's really cool is that we have an actual target for unisex contraceptive development," Miller said. "If you can stop progesterone from inducing a power stroke, sperm are not going to be able to reach or penetrate the oocyte."
While there are other possible targets for a contraceptive that would prevent the initiation of the power stroke, called hyperactivation, or the simultaneous release of enzymes that cut through the protective layer around the egg, "this is one of the better options we have for a unisex contraceptive," she said.
Senior author Polina Lishko, a UC Berkeley assistant professor of molecular and cell biology, noted that many tissues -- the brain, the lungs, smooth muscle -- contain related progesterone or steroid receptors that may work in a similar manner to trigger major changes in tissues.
"Now that we know the players, the next step is to look in other tissues that express these proteins to see whether progesterone acts on them in a similar manner to affect pain threshold adjustment in pain sensing neurons, surfactant production in the lungs or the excessive smooth muscle contractions found in asthma," she said. "This may be a universal pathway in all cells."
Miller, Lishko and their colleagues will publish their findings on March 17, 2016 in the journal Science.
Few known causes of male infertility
Today, doctors are unable to determine the cause of nearly 80 percent of all cases of male infertility, in part because little is known about the many molecular steps involved in the production of sperm and its interactions with the egg. Sperm may be to blame in half of all cases of infertile couples.
Yet because the U.S. government forbids the use of federal funds for research that brings eggs and sperm together in the same dish, little research has been done on how egg-sperm interactions lead to infertility. And until five years ago, it was very difficult to study the inner workings of sperm -- the body's smallest cell -- with ordinary lab techniques.
The new discovery comes thanks to techniques that Lishko and her colleague Yuriy Kirichok developed over the past five years at UCSF and UC Berkeley. The techniques allow them to stick electrodes on a sperm's tail and record its reactions to hormones, key to probing the molecular cascades that govern sperm behavior.
That technique led to their discovery that a large receptor on sperm tails -- a calcium channel dubbed CatSper -- is activated by progesterone from the egg. Progesterone unlocks the channel gate, letting electrically charged calcium atoms flood into the cell. This leads to a biochemical cascade that readies the sperm cell for its last-ditch effort to fertilize the oocyte.
Miller and Lishko suspected, however, that progesterone was not acting directly on the calcium channel, but on some other receptor that, in turn, activated the calcium channel.
That proved to be the case. They showed that progesterone actually binds to a previously mysterious enzyme called ABHD2, which is found at high levels in sperm. Once progesterone binds to the enzyme, which sits on the surface of the sperm, it removes a lipid (2AG) that has been inhibiting the calcium channel. Released of inhibition, CatSper opens the gate to calcium ions and eventual sperm activation.
The inhibitor of the calcium channel CatSper is probably there for a good reason: to prevent sperm from prematurely sprinting toward the egg and using up their limited supply of energy, Miller said.
"People tend to think of fertilization as like a marathon, where the fastest, most powerful sperm is going to win," Miller said. "We think of it like the Tour de France, where the riders in front are blocking the wind for the actual winner. Fertilization is a team sport, where the first sperm clear the way, expending their energy to break through the barrier cells, so that the slow and steady guy can get into the oocyte."
The study also sheds light on a long-standing mystery about steroids like progesterone: why they appear to act in two distinctly different ways. As a sex hormone, progesterone usually triggers a cascade of events in the cell that alter the expression of genes in the nucleus, a process that can take days. But sometimes progesterone causes immediate changes in the cell -- something called non-genomic steroid signaling -- that evidently use a quicker process than gene expression.
Lishko, who studies the sperm of rats, mice, bulls and boars as well as human to understand how fertilization works across different species, says that sperm are a perfect system in which to study non-genomic steroid signaling, since the genes in sperm are silenced and the normal type of steroid signaling is not present. As she and her colleagues uncover the basics of steroid signaling in sperm, the same process can then be studied in many other types of cells, she said.
source: University of California - Berkeley