Scientists at Nanyang Technological University, Singapore (NTU Singapore) have discovered that antibiotics can continue to be effective if bacteria's cell-to-cell communication and ability to latch on to each other are disrupted.
This research breakthrough is a major step forward in tackling the growing concern of antibiotic resistance, opening up new treatment options for doctors to help patients fight against chronic and persistent bacterial infections.
The study, led by Assistant Professor Yang Liang from the Singapore Centre for Environmental Life Sciences (SCELSE) at NTU, found that a community of bacteria, known as biofilm, can put up a strong line of defence to resist antibiotics. The NTU team has successfully demonstrated how biofilms can be disrupted to let antibiotics continue their good work.
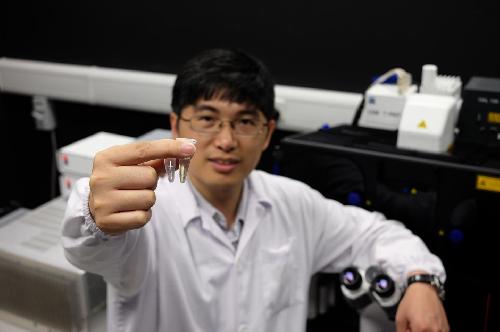 NTU Assistant Professor Yang Liang holding two drugs -- one disrupts biofilm while the other is an antibiotic that kills the bacteria. Credit: NTU Singapore
NTU Assistant Professor Yang Liang holding two drugs -- one disrupts biofilm while the other is an antibiotic that kills the bacteria. Credit: NTU Singapore
The research was published recently in Nature Communications, a prestigious academic journal by the Nature Publishing Group.
"Many types of bacteria that used to be easily killed by antibiotics have started to develop antibiotic resistance or tolerance, either through acquiring the antibiotic resistant genes or by forming biofilms," said Asst Prof Yang, who also teaches at NTU's School of Biological Sciences.
"The US Center for Disease Control estimates that over 60 per cent of all bacterial infections are related to biofilms. Our study has shown that by disrupting the cell-to-cell communication between bacteria and their ability to latch on to each other, we can compromise the biofilms, leaving the bacteria vulnerable and easily killed by antibiotics."
Bacterial resistance to antibiotics is rapidly growing world-wide and this puts at risk the ability to treat common infections in the community and hospitals.
The World Health Organisation states on its factsheet on Antimicrobial resistance that "without urgent, coordinated action, the world is heading towards a post-antibiotic era, in which common infections and minor injuries, which have been treatable for decades, can once again kill".
Associate Professor Kevin Pethe, an expert in antibiotic development and infectious diseases from NTU's Lee Kong Chian School of Medicine, said that this discovery may yield new treatment options that doctors can employ against chronic and persistent bacterial infections.
"Being able to disable biofilms and its protective benefits for the bacteria is a big step towards tackling the growing concern of antibiotic resistance," said Assoc Prof Pethe.
"While the scientific community is developing new types of antibiotics and antimicrobial treatments, this discovery may help to buy time by improving the effectiveness of older drugs."
How the discovery was made
Asst Prof Yang's team discovered the mechanisms of how bacteria are able to tolerate antibiotics by using a common bacterium Pseudomonas aeruginosa.
The bacteria were allowed to form a wall of biofilm in a microfluidic system. An antibiotic was then introduced. A large portion of the bacterial cells were killed by the antibiotic, leaving only a small fraction of antibiotic-tolerant cells. However, these cells were able to reproduce rapidly and dominate the community.
The scientists then used an FDA-approved drug that disrupts cell-to-cell communication (known as quorum sensing) and 'velcro'-like cells that can move and "stick" to each other. This drug was added to the antibiotic and together they managed to kill all the bacterial cells.
The same tests were then performed on mice with infected implants. It was found that only mice treated with a combination of anti-biofilm compound and antibiotics had their infections completely eradicated.
Interdisciplinary research
This discovery breakthrough was made possible through an interdisciplinary approach, where experts from three different fields - microbiology ecology, systems biology and chemical biology - came together to tackle the problem.
The NTU research team included proteomics expert Assoc Prof Newman Sze Siu Kwan from NTU's School of Biological Sciences. Proteomics was the key method used to discover chemical signals that bacterial cells in the biofilm use to communicate with each other.
Another researcher in the team is Professor Michael Givskov, a world-leading scientist in the area of biofilm research and bacterial cell-to-cell communication at SCELSE. Together, the team found that traditional methods of isolating the bacteria from the biofilm for observation did not work, as the bacteria behave differently after being isolated from the biofilm.
This study, supported by the Ministry of Education Academic Research Fund, took Asst Prof Yang and his team four years to complete. Moving forward, they will seek more ways to improve efficiency of antibiotics for persistent infections.
"What we hope to do is to develop new compounds that are able to better target biofilms. This will help existing drugs perform better at overcoming biofilm infections, which is commonly seen in cases of patients with artificial implants and chronic wounds, as they have very limited effective treatment options that are effective," said Asst Prof Yang.
source: Nanyang Technological University