A common flu virus could be used to overcome patients' resistance to certain cancer drugs -- and improve how those drugs kill cancer cells, according to new research from Queen Mary University of London (QMUL).
The work, funded by UK charity Pancreatic Cancer Research Fund, contributes to a growing area in cancer treatment in which viruses are harnessed to kill cancer cells.
Viruses can be modified to specifically infect cancer cells, and use them as a factory to generate thousands of new viruses, replicating until the cancer cell bursts. The virus copies will then spread and infect surrounding tumour cells and repeat the process, leaving healthy cells unharmed.
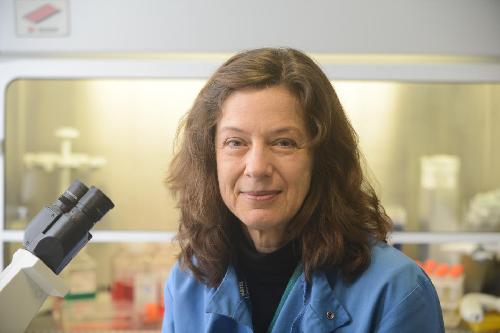 This is a picture of Dr. Gunnel Hallden, Barts Cancer Institute, QMUL. Credit: Pancreatic Cancer Research Fund
This is a picture of Dr. Gunnel Hallden, Barts Cancer Institute, QMUL. Credit: Pancreatic Cancer Research Fund
But the body's immune system will usually kill off the virus before it is able to infect all the cells within a tumour. In pancreatic cancer, therefore, drugs such as gemcitabine are currently the most common treatment -- they work by damaging the DNA in the cancer cells, so they are unable to divide successfully. This damage triggers a process called apoptosis, in which damaged or unhealthy cells are forced to self-destruct.
Over time, however, the cancer cell becomes able to delay apoptosis in order to repair the damage to its DNA, which means that the cells survive and continue to divide and spread and the drug becomes less effective.
In a study published in the journal Oncotarget, the team at QMUL's Barts Cancer Institute introduced a genetic modification to the virus, called adenovirus, to give it an extra weapon against cancer cells.
By switching off a particular gene in the virus which counteracts apoptosis, the scientists found cancer cells studied in the laboratory were unable to delay apoptosis and so forced to die without dividing. The modified virus still infects some cancer cells and replicates until the cell bursts, but by also preventing the cancer cells from developing drug resistance, it works with the anti-cancer drug to increase the number of cells that are killed.
"Many cancers -- including pancreatic cancer -- become resistant to treatments like gemcitabine, and currently there's no way to get round that," explains Dr Gunnel Halldèn, who led the research. "The virus that we have modified re-sensitises the resistant cancer cell by preventing the cell from repairing itself. The virus alone will kill some tumour cells, but in combination with the drug, the number of cells that are killed is greatly increased.
"Because the virus improves the efficacy of the drug, it means it could also be possible to give lower doses, which will also reduce the unpleasant side-effects associated with chemotherapy," she adds.
Developing virus-based cancer therapies has been a key goal in cancer research for several years and some technologies have already moved into the clinic: last year, for example, a melanoma therapy, based on a herpes virus called T-VEC, was approved for use in the US and in Europe.
The QMUL research is at an early stage, but the team believe they have found a promising new route for developing combination treatments for pancreatic cancer.
The next step for the researchers will be to test other modified versions of adenovirus to better understand the exact mechanism through which it enhances cell killing. Further modifications will also be made to enable the virus to trigger the body's immune system, which will attack any cancer cells that have not been infected by the virus.
source: Pancreatic Cancer Research Fund