One in three people world-wide are thought to be infected with Mycobacterium tuberculosis (Mtb), but most remain well because their immune system keeps the pathogen in check. HIV infection dramatically increases the risk of Mtb infection turning into active tuberculosis (TB), a life-threatening disease. Exactly how HIV infection affects the immune system's ability to suppress active TB is still poorly understood.
A study published on March 17th in PLOS Pathogens suggests that it is not a general weakening of the immune system by HIV that initially leads to loss of Mtb control, but rather that HIV is associated with a failure to prevent harmful immune responses. As HIV disease progresses, the weakening immune system's focus on antiviral responses leaves it largely defenseless against the Mtb pathogen.
Mahdad Noursadeghi, from University College London, UK, and colleagues, performed a detailed analysis of the immune response to Mtb in individuals at different stages of HIV infection. They used the standard tuberculin skin test (TST), a sterile injection of purified Mtb proteins into the forearm skin, and then measured the activity of all possible genes in the injection-site tissue of volunteer participants 48 hours later, to characterize the immune response in comprehensive detail.
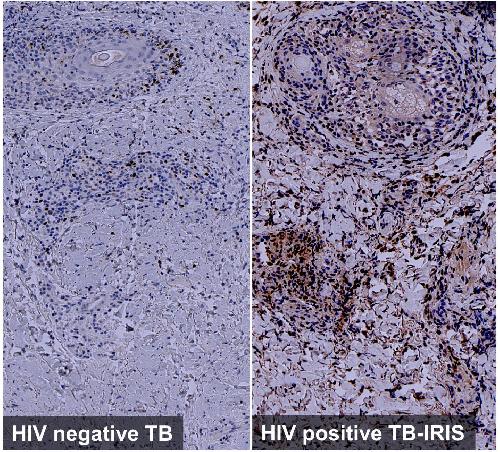 This image shows exaggerated IRF4 expression associated with Th2 immunity in tuberculin skin tests of HIV infected TB-IRIS patients. Credit: Lucy Bell, University College London
This image shows exaggerated IRF4 expression associated with Th2 immunity in tuberculin skin tests of HIV infected TB-IRIS patients. Credit: Lucy Bell, University College London
The researchers started with HIV-negative volunteers who had active TB, and found a specific TST gene signature produced in response to the injection. They then compared the TST signature with published gene expression profiles from active TB disease sites in the lung, as well as with gene expression patterns in the circulating blood from active TB patients. They found that the gene expression changes within the TST more accurately reproduced the molecular patterns at the site of active TB than the changes in peripheral blood, and used this to quantify immune cell recruitment and a wide range of other specific immune responses.
To investigate the effects of HIV, the researchers compared the HIV-negative TST signatures with those from HIV-positive patients with active TB, and found that a predominant effect of early HIV infection was to diminish a specific component of the immune response called IL-10 that usually dampens harmful inflammation. In more advanced HIV, they found almost no protective immune response to Mtb. Instead they observed isolated interferon responses which are usually involved in anti viral protection, but may also weaken anti-TB defenses.
When patients start anti-HIV medication, some individuals co-infected with HIV and Mtb develop a dangerous condition called TB-IRIS ('immune reconstitution inflammatory syndrome'). As the immune system of such patients recovers, it responds to Mtb with an overwhelming inflammatory response that can be life-threatening. When the researchers studied the TST profile in these patients, they found that most parts of the immune system had recovered to normal levels, but that the balance was disrupted because a particular type of immune response, called Th2-type immunity, that is associated with asthma and allergies, was much stronger than normal.
"Using transcriptional profiling of the TST", the researchers conclude, they "identified novel and diverse molecular mechanisms by which human immune responses to Mtb are dysregulated in HIV co-infected patients". If validated by additional studies, they hope that their results advance the development of new therapies for TB by modifying immune responses.
source: PLOS