Tsukuba, Japan - Researchers have thus far been unable to comprehensively explain how various factors regulate the size of a population of regulatory T (Treg) immune cells, which influence other immune system components and affect inflammation. However, as recently reported in an article published online in Nature Immunology, a team of researchers based at the University of Tsukuba have now shown how beneficial bacteria in the gut can help Treg cells to proliferate, but that dying epithelial cells suppress this effect.
This latest work builds on previous studies that have shown that beneficial bacteria, known as commensals, can modulate tissue status, including the effect they have on Treg cells. These cells are known to regulate immune activity, but details on this mechanism have never been clear. This issue is especially significant at barrier surfaces, such as in the gastrointestinal tract, where large numbers of epithelial cells detach and die via apoptosis. Prior to this study, it had also been unclear whether these dying cells had any particular effects.
Through a range of experiments, the research group showed that these dying, or apoptotic, cells in fact work to suppress proliferation of Treg cells. This is normally promoted by beneficial bacteria in the gut. The group also specifically identified the molecules involved--information that could be useful for treating diseases in which Treg cells are involved or are dysfunctional.
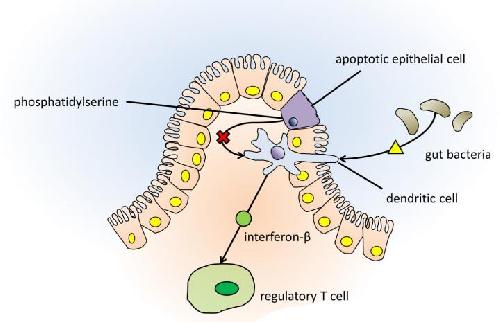 Gut bacteria interact with dendritic cells to increase production of interferon-β, which in turn stimulates regulatory T cell production. Apoptotic epithelial cells can also interact with dendritic cells, reducing the amount of interferon-β produced, controlling regulatory T cell production. Credit: University of Tsukuba
Gut bacteria interact with dendritic cells to increase production of interferon-β, which in turn stimulates regulatory T cell production. Apoptotic epithelial cells can also interact with dendritic cells, reducing the amount of interferon-β produced, controlling regulatory T cell production. Credit: University of Tsukuba
"This is truly an important study because it shows that these apoptotic epithelial cells are not just waste for the body to rid itself of, but instead actively influence their environment within the gut," says corresponding author Akira Shibuya of the University of Tsukuba's Department of Immunology. "Also interesting is that that the immune cell dendritic cells are mediators of the effects of commensal bacteria promoting Treg cell proliferation, yet apoptotic epithelial cells can block this action using phosphatidylserine on their surfaces."
By disabling a gene expressed on dendritic cells in mice, the Treg cell population size increased markedly. The researchers thus realized this gene normally suppresses Treg cell proliferation. The product this gene encodes interacts with phosphatidylserine on apoptotic epithelial cells, which blocks production of the signaling molecule interferon-ß by dendritic cells, thereby preventing Treg cell proliferation.
"The potential benefits of our findings are suggested by the differences between a group of normal mice and a group of mice in which the receptor for apoptotic epithelial cell-derived phosphatidylserine was knocked out," first author Chigusa Nakahashi-Oda says. "When these effects due to dying epithelial cells couldn't occur, there was less severe inflammation of the colon after a damaging treatment, and in another experiment there was decreased skin and airway inflammation in mice."
Now that the different molecules involved in this immune system pathway are known, it is hoped that researchers will be able to target them in order to treat diseases associated with Treg cells, such as inflammatory and allergic diseases.
source: University of Tsukuba