DURHAM, N.C. -- A Duke research team has developed a better recipe for synthetic replacement cartilage in joints.
Combining two innovative technologies they each helped develop, lead authors Farshid Guilak, a professor of orthopedic surgery and biomedical engineering, and Xuanhe Zhao, assistant professor of mechanical engineering and materials science, found a way to create artificial replacement tissue that mimics both the strength and suppleness of native cartilage. Their results appear Dec. 17 in the journal Advanced Functional Materials.
Articular cartilage is the tissue on the ends of bones where they meet at joints in the body – including in the knees, shoulders and hips. It can erode over time or be damaged by injury or overuse, causing pain and lack of mobility. While replacing the tissue could bring relief to millions, replicating the properties of native cartilage -- which is strong and load-bearing, yet smooth and cushiony -- has proven a challenge.
In 2007 Guilak and his team developed a three-dimensional fabric "scaffold" into which stem cells could be injected and successfully "grown" into articular cartilage tissue. Constructed of minuscule woven fibers, each of the scaffold's seven layers is about as thick as a human hair. The finished product is about 1 millimeter thick.
Since then, the challenge has been to develop the right medium to fill the empty spaces of the scaffold -- one that can sustain compressive loads, provide a lubricating surface and potentially support the growth of stem cells on the scaffold. Materials supple enough to simulate native cartilage have been too squishy and fragile to grow in a joint and withstand loading. "Think Jell-O," says Guilak. Stronger substances, on the other hand, haven't been smooth and flexible enough.
That's where the partnership with Zhao comes in.
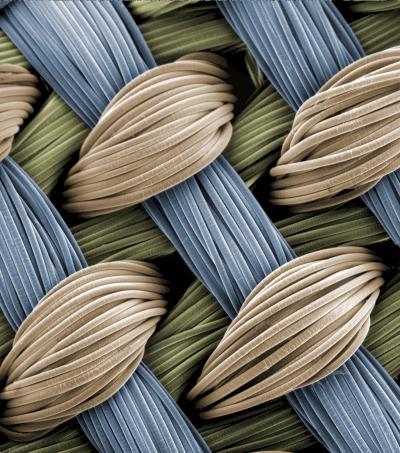
Tiny interwoven fibers make up the three-dimensional fabric "scaffold" into which a strong, pliable hydrogel is integrated and injected with stem cells, forming a framework for growing cartilage. This image appears on the cover of the Dec. 17, 2013, issue of Advanced Functional Materials.
(Photo Credit: courtesy of Frank Moutos and Farshid Guilak)
Zhao proposed a theory for the design of durable hydrogels (water-based polymer gels) and in 2012 collaborated with a team from Harvard University to develop an exceptionally strong yet pliable interpenetrating-network hydrogel.
"It's extremely tough, flexible and formable, yet highly lubricating," Zhao says. "It has all the mechanical properties of native cartilage and can withstand wear and tear without fracturing."
He and Guilak began working together to integrate the hydrogel into the fabric of the 3-D woven scaffolds in a process Zhao compares to pouring concrete over a steel framework.
In their experiments, the researchers compared the resulting composite material to other combinations of Guilak's scaffolding embedded with previously studied hydrogels. The tests showed that Zhao's invention was tougher than the competition with a lower coefficient of friction. And though the resulting material did not quite meet the standards of natural cartilage, it easily outperformed all other known potential artificial replacements across the board, including the hydrogel and scaffolding by themselves.
"From a mechanical standpoint, this technology remedies the issues that other types of synthetic cartilage have had," says Zhao, founder of Duke's Soft Active Materials (SAMs) Laboratory. "It's a very promising candidate for artificial cartilage in the future."
The team's next step will likely be to implant small patches of the synthetic cartilage in animal models, according to Guilak and Zhao.
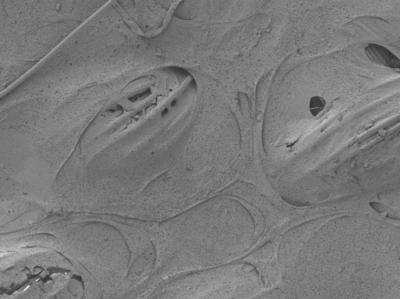
This is a closer look at the scaffolding integrated with Xuanhe Zhao's hydrogel. The composite material, formed through a process comparable to pouring concrete over a steel framework, may be a serviceable synthetic replacement for the load-bearing cartilage found between bones.
(Photo Credit: courtesy of I-Chien Liao, Frank Moutos, Brad Estes)
Source: Duke University