It took just 16 two-hour classes on the basics of a healthy lifestyle to substantially reduce cardiovascular risks associated with type 2 diabetes and elevated fasting blood glucose levels for 110 patients, according to a study published in The Journal of the American Osteopathic Association.
The Complete Health Improvement Lifestyle Intervention Program (CHIP) includes dietary targets, cooking classes, an exercise program and group discussions to give participants the specifics they need to improve their health. Based on the fact that 75 percent or more of Western diseases are lifestyle-related, CHIP gives participants concrete instruction that takes a mind, body and spirit approach to healthy living.
The retrospective study evaluated 2011-2014 data collected from 110 patients in six Ohio University CHIP cohorts from 11 Appalachian counties where the prevalence of diabetes is over 7 percent higher than the national average. Participants experienced significant reductions in total cholesterol levels (9.6 percent), fasting glucose (9 percent), body mass index (3.7 percent) and systolic blood pressure (5.7 percent). (See data table)
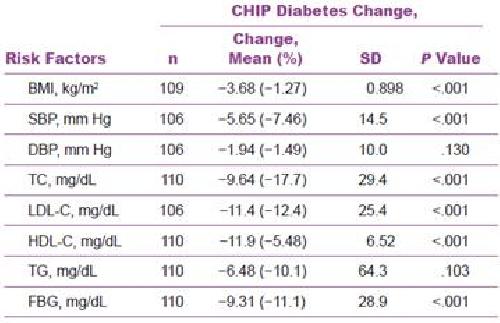 The JAOA study evaluated 2011-2014 data collected from 110 patients in six Ohio University CHIP cohorts from 11 Appalachian counties where the prevalence of diabetes is over 7 percent higher than the national average. Participants experienced significant reductions in total cholesterol levels (9.6 percent), fasting glucose (9 percent), body mass index (3.7 percent) and systolic blood pressure (5.7 percent). Credit: Journal of the American Osteopathic Association
The JAOA study evaluated 2011-2014 data collected from 110 patients in six Ohio University CHIP cohorts from 11 Appalachian counties where the prevalence of diabetes is over 7 percent higher than the national average. Participants experienced significant reductions in total cholesterol levels (9.6 percent), fasting glucose (9 percent), body mass index (3.7 percent) and systolic blood pressure (5.7 percent). Credit: Journal of the American Osteopathic Association
"This study supports the osteopathic philosophy of medicine, including that diet and exercise are the most effective prescriptions physicians can give patients struggling with lifestyle diseases like Type 2 diabetes. But lifestyle changes require more commitment than taking a pill, which is why programs like CHIP are so beneficial," said Jay Shubrook, DO, a diabetologist at Touro University California, College of Osteopathic Medicine in Vallejo. "Community-based interventions provide the social supports and specific instruction that move patients into healthy habits, which in some cases enabled them to reduce medications."
The primary focus of CHIP was the consumption of whole foods, such as fresh fruits, vegetables, whole grains, legumes, nuts, and 8 ten-oz glasses of water daily. More specific goals included overall dietary fat content below 20 percent of total calories, daily intake of added sugar less than 10 tsp, daily sodium less than 2000 mg, choles¬terol below 50 mg, and high fiber intake (>35 g/d). Stress reduction techniques and flexibility exercises were taught and encouraged, along with at least 30 minutes (or 10,000 steps) of daily aerobic exercise.
Currently almost 30 million Americans have diabetes and 1 in 3 Americans have prediabetes. Diabetes complications include cardiovascular disease, stroke, limb amputation and microvascular complications. Direct medical costs for diabetes in the U.S. are estimated at $176 billion annually. Indirect costs from disability, work lost and premature death add up to another $69 billion.
To date, CHIP has shown to be effective in maintaining reductions in CVD risk factors for up to three years after completion of the program.
"This program engages the community to strive for and reach better health, while preparing participants with the structure they need to continue a healthy lifestyle in the future," Shubrook explained.
source: American Osteopathic Association