A group of researchers led by Dr. James Dunn out of the University of California, Los Angeles (UCLA) are pleased to announce publication of their research in an upcoming issue of the journal TECHNOLOGY. The report, part of a thesis project of first author Christopher Walthers, Ph.D, was co-authored by Chase Lyall, M.S., Alireza Nazemi, M.S., and Puneet Rana, M.S.
This paper describes methods to optimize characteristics of cells grown in a lab using biomaterial coatings. Dr. Dunn's research falls within the field of tissue engineering - the use of biomaterials, cells, and natural factors to regenerate tissues and organs lost to disease or injury. Dr. Dunn's group has used a biodegradable polymer coated with two common biomaterials--collagen and heparan sulfate--to emphasize differences in cell-material interactions in different environments.
Specifically, smooth muscle cells from rat intestine were grown on the polymer after coating with either collagen or heparan sulfate and either grown continually in the lab or implanted in a rat. It is common in tissue engineering applications to grow cells in a lab prior to implantation to increase cell numbers in a controlled environment. Collagen is a common tissue engineering biomaterial often used to aid cell attachment and growth in culture. While collagen-coated implants allowed for greater cell growth in the lab, heparan sulfate-coated implants allowed for greater cell growth and survival after implantation by spurring development of blood vessels.
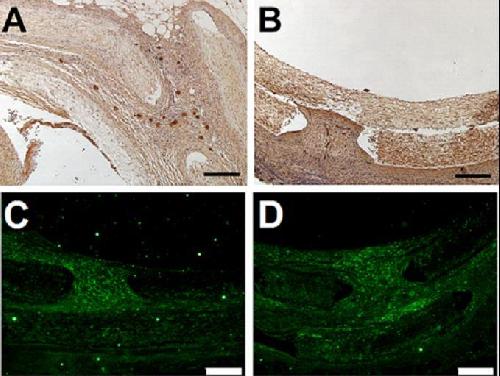 Implants with heparan sulfate-coating showed an increase in blood vessel infiltration (A) compared to collagen-coated implants (B) with staining for von-Willebrand Factor (dark brown dots). Implants showed similar numbers of implanted smooth muscle cells (stained green) whether they were coated with heparan sulfate (C) or collagen (D) despite the significant decrease in cell numbers to attach and grow initially on heparan sulfate-coated implants in culture. Credit: TECHNOLOGY
Implants with heparan sulfate-coating showed an increase in blood vessel infiltration (A) compared to collagen-coated implants (B) with staining for von-Willebrand Factor (dark brown dots). Implants showed similar numbers of implanted smooth muscle cells (stained green) whether they were coated with heparan sulfate (C) or collagen (D) despite the significant decrease in cell numbers to attach and grow initially on heparan sulfate-coated implants in culture. Credit: TECHNOLOGY
"We were surprised to see how well heparan sulfate-coated implants improved cell survival after implantation. We knew that heparan sulfate increases blood vessel development from the research of an earlier Ph.D student, Dr. Shivani Singh, but we didn't expect to see such a drastic change in survival of the cells. Heparan sulfate is a very interesting molecule and we are excited to learn more about how it interacts with growth factors in the body," said Dr. Walthers, lead author on the paper.
Dr. Dunn's lab has focused on generating functional tissues of the digestive tract to treat diseases primarily affecting pediatric patients, namely short bowel syndrome. In these patients, there is insufficient intestine to digest and absorb adequate nutrition. More traditional treatments like intestinal transplantation are complicated by a number of undesirable side-effects, making tissue engineering an interesting alternative. A functional tissue-engineered intestine would need to be similar in thickness and strength to normal intestinal muscle to make it a viable treatment for short bowel syndrome. "Improving the number of smooth muscle cells that can survive and grow after transplantation of an engineered tissue would bring us one step closer to a fully functional tissue-engineered intestine for short bowel syndrome," said Dr. Walthers.
Future applications of this research could seek to emphasize properties of heparan sulfate that increase blood vessel development to improve engineered tissues and organs, for example by injecting heparan sulfate during implantation or by attaching important segments of heparan sulfate on the surfaces of engineered tissues. The group is now exploring related areas of intestinal tissue engineering, including developing the absorptive epithelial cells that line the inside of the tissue, increasing contraction strength of smooth muscle cells grown in the lab, and making a model "organ on a chip" of intestinal smooth muscle to study in the lab.
source: World Scientific