Smoking increases an individual's risk of developing tuberculosis (TB) - and makes the infection worse - because it causes vital immune cells to become clogged up, slowing their movement and impeding their ability to fight infection, according to new research published in the journal Cell.
TB is an infectious disease caused by Mycobacterium tuberculosis that primarily infects the lungs, but can also infect other organs. It is transmitted from person to person through the air. The disease can cause breathlessness, wasting, and eventual death. While treatments do exist, the drug regimen is one of the longest for any curable disease: a patient will typically need to take medication for six months.
For people exposed to TB, the biggest risk factor for infection is exposure to smoke, including active and passive cigarette smoking and smoke from burning fuels. This risk is even greater than co-infection with HIV. However, until now it has not been clear why smoke should increase this risk.
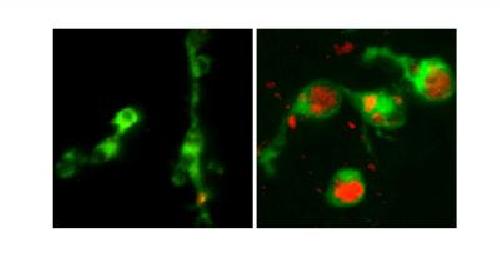 Left: normal macrophages (green)Right: dysfunctional macrophages whose lysosomes (red) are clogged with cell debris. Credit: Steven Levitte, Lalita Ramakrishnan
Left: normal macrophages (green)Right: dysfunctional macrophages whose lysosomes (red) are clogged with cell debris. Credit: Steven Levitte, Lalita Ramakrishnan
When TB enters the body, the first line of defence it encounters is a specialist immune cell known as a macrophage (Greek for 'big eater'). This cell engulfs the bacterium and tries to break it down. In many cases, the macrophage is successful and kills the bacterium, preventing TB infection, but in some cases TB manages not just to avoid destruction, but to use macrophages as 'taxi cabs' and get deep into the host, spreading the infection. TB's next step is to cause infected macrophages to form tightly-organised clusters known as tubercles, or granulomas. Once again here, the macrophages and bacteria fight a battle - if the macrophages lose, the bacteria use their advantage to spread from cell to cell within this structure.
An international team of researchers, led by the University of Cambridge, and the University of Washington, Seattle, studying genetic variants that increase susceptibility to TB in zebrafish - a 'see-through' animal model for studying the disease - identified a variant linked to 'lysosomal deficiency disorders'. The lysosome is a key component of macrophages responsible for destroying bacteria. This particular variant caused a deficiency in an enzyme known as cathepsin, which acts within the lysosome like scissors to 'chop up' bacteria; however, this would not necessarily explain why the macrophages could not destroy the bacteria, as many additional enzymes could take cathepsin's place.
The key, the researchers found, lay in a second property of the macrophage: housekeeping. As well as destroying bacteria, the macrophage also recycles unwanted material from within the body for reuse, and these lysosomal deficiency disorders were preventing this essential operation.
Professor Lalita Ramakrishnan from the Department of Medicine at the University of Cambridge, who led the research, explains: "Macrophages act a bit like vacuum cleaners, hoovering up debris and unwanted material within the body, including the billions of cells that die each day as part of natural turnover. But the defective macrophages are unable to recycle this debris and get clogged up, growing bigger and fatter and less able to move around and clear up other material.
"This can become a problem in TB because once the TB granuloma forms, the host's best bet is to send in more macrophages at a slow steady pace to help the already infected macrophages."
"When these distended macrophages can't move into the TB granuloma," adds co-author Steven Levitte from the University of Washington, "the infected macrophages that are already in there burst, leaving a 'soup' in which the bacteria can grow and spread further, making the infection worse."
The researchers looked at whether the effect seen in the lysosomal deficiency disorders, where the clogged-up macrophage could no longer perform its work, would also be observed if the lysosome became clogged up with non-biological material. By 'infecting' the zebrafish with microscopic plastic beads, they were able to replicate this effect.
"We saw that accumulation of material inside of macrophages by many different means, both genetic and acquired, led the same result: macrophages that could not respond to infection," explains co-author Russell Berg.
This discovery then led the team to see whether the same phenomenon occurred in humans. Working with Professor Joe Keane and his colleagues from Trinity College Dublin, the researchers were able to show that the macrophages of smokers were similarly clogged up with smoke particles, helping explain why people exposed to smoke were at a greater risk of TB infection.
"Macrophages are our best shot at getting rid of TB, so if they are slowed down by smoke particles, their ability to fight infection is going to be greatly reduced," says Professor Keane. "We know that exposure to cigarette smoke or smoke from burning wood and coal, for example, are major risk factors for developing TB, and our finding helps explain why this is the case. The good news is that stopping smoking reduces the risk - it allows the impaired macrophages to die away and be replaced by new, agile cells."
source: University of Cambridge