Frozen sperm taken by biopsy from testicles in men with no sperm in their semen is as effective as fresh sperm taken by biopsy in helping couples conceive through in vitro fertilization (IVF), according to a study at Washington University School of Medicine in St. Louis.
The researchers also determined that the type of facility where sperm is taken and its distance from the IVF laboratory has no bearing on pregnancy outcomes.
The findings, published online in PLOS ONE, may benefit men with no sperm in their semen due to genetics, cancer diagnoses or testicular failure. These men do not have enough sperm to have their own children through IVF without being biopsied.
In these men, a biopsy in a testicle often results in enough sperm to be used in a procedure called intracytoplasmic sperm injection (ICSI) as part of the IVF process in men with severe infertility.
The biopsy, which is usually performed on an outpatient basis, involves obtaining tissue from testicles that is examined for sperm. If sperm are found, they are removed and used immediately in ICSI or frozen for future use.
In ICSI, a single sperm is injected into an egg that has been surgically retrieved from a woman's ovaries. The fertilized egg, or embryo, then is transferred to the woman's womb.
"The convenience and ease of being able to use frozen sperm taken by biopsy in ICSI offers many advantages over fresh sperm," said Kenan Omurtag, MD, the study's first author and assistant professor of obstetrics and gynecology."
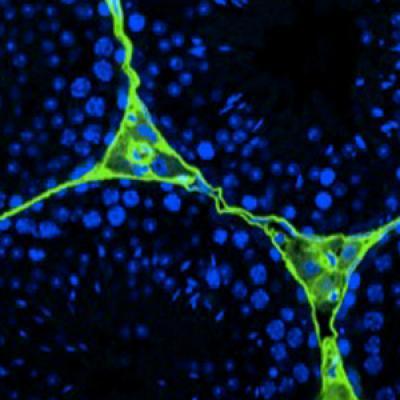
Pictured is a section of human testicular tissue and sperm cells under confocal microscopy.
(Photo Credit: Erica Schoeller)
When fresh sperm is used, the biopsy for the sperm retrieval needs to be done the day before or on the same day as egg retrieval from the woman, and this may not be convenient for the couple. When frozen sperm is used, the man can have his biopsy first, and if sperm is found, it can be banked. Then, at the couple's convenience, the woman's eggs are retrieved and ICSI can be completed.
Before ICSI, a woman takes daily injections of fertility medications for a week to 10 days to stimulate her ovaries to produce eggs. Using an ultrasound to locate eggs, a doctor then removes them from the woman's ovaries with a fine, hollow needle.
In this study, researchers analyzed data from 1995 through 2009 from the Washington University Infertility and Reproductive Medicine Center.
One hundred thirty-six men had testicular biopsies to be used in ICSI. Of those biopsies, 84 percent involved frozen sperm and the remaining 16 percent used fresh sperm. A statistically significant difference in fertilization rate was noted between frozen sperm (62 percent) and fresh (47 percent) sperm, respectively. There was no difference between the delivery rate.
Two urologists performed 150 testicular sperm biopsies in an operating room adjacent to the IVF lab, in an operating room in another building almost one mile from the IVF lab and in an ambulatory surgical center about 15 miles from the IVF lab. The maximum travel time from the third site was less than 30 minutes.
There was no statistically significant difference between the locations and pregnancy results.
"Men with no sperm in their semen now have more options to have children of their own," said Randall Odem, MD, co-author of the study and professor of obstetrics and gynecology, who recommends that men with infertility issues seek treatment from a reproductive endocrinologist and a urologist trained in male infertility.
"This study demonstrates that using frozen sperm taken by biopsy works as well for most patients in what matters most —pregnancy rates," he said.